Tauopathy and neurodegeneration
Neurodegenerative diseases are a growing public health concern globally, with significant impacts on both the patients and the healthcare systems that aid them. Among them, tauopathies present one of the greatest challenges, encompassing approximately 20 progressive and fatal disorders, including Alzheimer’s disease, progressive supranuclear palsy, and corticobasal degeneration. Tauopathies are characterized by the abnormal accumulation of hyper-phosphorylated tau protein in the brain; these tau aggregates spread between neurons, causing neuronal loss and cognitive decline. Despite extensive research, it is still unclear how these aggregates drive cellular toxicity and disease progression. The structural complexity of tau and the mechanism of its aggregation has made therapeutic development particularly challenging.
The prevalence and impact of tauopathies
Among tauopathies, Alzheimer’s disease is the most widespread, accounting for approximately 60–70% of all dementia cases globally. As of 2019, over 57 million people were affected by Alzheimer’s and other dementias, a number projected to rise to 153 million by 2050.1 The primary hallmarks of Alzheimer’s pathology are intracellular tau tangles and extracellular amyloid-β (Aβ) plaques. Though comprehensively investigated, their precise molecular architecture, localization, interactors, and propagation mechanisms remain elusive. Understanding the structural basis of these aggregates is crucial for developing diagnostic markers and disease-modifying treatments. For example, epigallocatechin gallate (EGCG), a compound found in green tea, has been shown to disaggregate tau and Aβ fibrils. However, its poor bioavailability highlights the necessity of structure-based drug design for more effective therapeutics.2
Cryo-EM: a game changer in tauopathy research
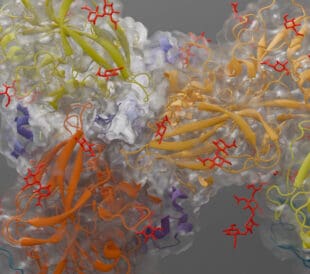
Cryo-electron microscopy (cryo-EM) advancements have revolutionized tauopathy research by enabling near-atomic resolution visualization of tau structures in apo and ligand-bound forms (Figure 1).3 These studies have revealed that synthetic tau aggregates differ structurally from those extracted from human brains impacted by Alzheimer’s disease.4 Cryo-EM studies of human tau filaments have enabled the classification of tauopathies based on their unique folds, underscoring the importance of human-brain-derived aggregates for translationally relevant research.5 However, these findings are primarily based on extracted tau filaments, leaving gaps in our understanding of tau behavior within the native cellular context. Investigating tau in situ is therefore crucial for the design of improved diagnostic and treatment strategies.

Figure 1. Cryo-EM electron density map (gray) and structural model (magenta) of tau paired helical filaments found in the extracellular vesicles of brains afflicted by Alzheimer’s disease. Figure adapted from Fowler et al. under CC BY 4.0.
Cryo-electron tomography: unlocking the native state of tau aggregates
Cryo-electron tomography (cryo-ET) provides high-resolution, 3D imaging of biological molecules in their native, hydrated state. Unlike conventional electron microscopy, cryo-ET preserves ultrastructural details without staining or fixation. This technique, combined with sub-tomogram averaging, enhances our understanding of the molecular architecture underlying Alzheimer’s pathology. By visualizing tau and Aβ aggregates in human brain tissue, cryo-ET can bridge the gap between in vitro models and actual disease pathology, aiding in therapeutic development.
Deciphering Aβ architecture in mouse brain tissue
The amyloid-β plaques found in knock-in mouse models of familial Alzheimer’s disease form a highly complex fibrillar network. They contain fully assembled fibrils, protofilament-like rods, and branched fibrils, suggesting secondary nucleation mechanisms. They are also interwoven with extracellular vesicles, multilamellar bodies, and other subcellular structures, emphasizing their heterogeneous composition.6
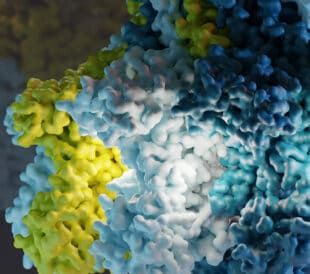
Investigation of naturally occurring Aβ mutations reveals additional details on how the protein aggregates and functions. For instance, the Arctic (E22G) Aβ variant has demonstrated altered fibril folds that affect core residues and protofilament arrangement. This structural variation could explain why Pittsburgh B, a PET imaging tracer, fails to detect Arctic Aβ aggregates in both human patients and animal models. Differences in fibril width and regional thickness between in-tissue and ex-vivo structures of Arctic Aβ fibrils have also been observed (Figure 2).6

Figure 2. Fibril composed of Arctic Aβ mutant, taken from a mouse model. These fibrils exhibit differences in width and branching pattern in-tissue, as compared to ex-vivo. Figure adapted from Leistner et al. under CC BY 4.0.
These findings carry significant implications for immunotherapies targeting Aβ. Current antibody designs may not effectively recognize structurally distinct fibrils, potentially limiting their efficacy. The structural insights from this study contribute to a more comprehensive model of amyloid-β plaque formation. Further research utilizing postmortem human brain tissue is, however, required to fully understand whether these observations, obtained in vitro and from model organisms, truly align with disease behavior in vivo.
Mapping tauopathy structures in human brain tissue
Cryo-ET has made it possible to view tau structures in human brain tissue under near-native conditions. Unlike conventional techniques that require chemical fixation or staining, cryo-ET allows researchers to study tau filaments in their natural cellular environment.7

Figure 3. Tomographic slices of human brain tissue showing pathological features, including Aβ plaques (left, cyan) and tau filaments (right, yellow). Figure adapted from Gilbert et al. under CC BY 4.0.
A recent study by Gilbert et al. showcases the unprecedented insights that can be obtained with this technique, revealing the structural organization of intercellular Aβ and intracellular tau filaments in postmortem samples obtained from Alzheimer’s patients.8 These studies showed that Aβ plaques exhibit a lattice-like structure interwoven with extracellular vesicles and cuboidal particles—components absent in healthy brain tissue (Figure 3). Branched Aβ fibrils and proto-filament-like rods were also observed, suggesting that secondary nucleation mechanisms play a role in plaque development.

Figure 4. In postmortem brain samples from Alzheimer’s patients, tau exists as either a mixture of paired helical filaments and straight filaments, or as straight filaments only. Figure adapted from Gilbert et al. under CC BY 4.0
Unlike Aβ, tau filaments in these tissue samples appear as parallel, unbranched structures that are clustered together, potentially due to cellular constraints or lateral interactions. The structural variation of tau filaments across different brain regions further highlights the spatial heterogeneity of Alzheimer’s pathology (Figure 4). These findings reinforce the complexity of tauopathies and emphasize the necessity of studying disease mechanisms in their native environment.
Paving the way for precision medicine in Alzheimer’s disease and other tauopathies
High-resolution imaging of Alzheimer’s disease samples has revealed critical structural variations in tau filaments, the impact of mutations on Aβ structure, and the presence of non-amyloid components that may modulate disease progression. These findings deepen our understanding of Alzheimer’s pathology; with a clearer picture of how Aβ and tau aggregates form and interact with their surroundings, the field is moving closer to precision medicine for Alzheimer’s disease.
In addition to disease investigation and treatment, these studies could help us redefine laboratory models of tauopathies and other neurodegenerative diseases, as current models often fail to fully represent human pathology, leading to limited translational success. By integrating in situ structural insights, researchers can develop more physiologically relevant models that accurately reflect disease conditions in patients.
Future studies of tauopathies and other protein misfolding disorders will benefit greatly from similar investigations on postmortem brain tissue, providing otherwise inaccessible insights into disease-specific protein assemblies. This information will be crucial for understanding disease mechanisms, designing targeted diagnostic and therapeutic compounds, and refining lab models used to study tauopathies.
References
- GBD 2019 Dementia Forecasting Collaborators. Estimation of the global prevalence of dementia in 2019 and forecasted prevalence in 2050: an analysis for the Global Burden of Disease Study 2019. The Lancet Public Health 7:2, e105–125 (2022). doi: 1016/S2468-2667(21)00249-8
- Seidler, PM, et al.Structure-based discovery of small molecules that disaggregate Alzheimer’s disease tissue derived tau fibrils in vitro. Nat Commun 13:5451 (2022). doi: 1038/s41467-022-32951-4
- Fowler, SL, et al. Tau filaments are tethered within brain extracellular vesicles in Alzheimer’s disease. Nature Neuroscience 28, 40-48 (2025). doi: 1038/s41593-024-01801-5
- Yang, Y, et al. Cryo-EM structures of amyloid-β 42 filaments from human brains. Science 375:6577 (2022). doi: https://doi.org/10.1126/science.abm7285
- Shi, Y, et al. Structure-based classification of tauopathies. Nature 598, 359–363 (2021). doi: 1038/s41586-021-03911-7
- Leistner, C, et al. The in-tissue molecular architecture of β-amyloid pathology in the mammalian brain. Nat Commun 14:2833 (2023). doi: 1038/s41467-023-38495-5
- Creekmore, BC, et al.Ultrastructure of human brain tissue vitrified from autopsy revealed by cryo-ET with cryo-plasma FIB milling. Nat Commun 15:2660 (2024). doi: 1038/s41467-024-47066-1
- Gilbert, MAG, et al. CryoET of β-amyloid and tau within postmortem Alzheimer’s disease brain. Nature 631, 913–919 (2024). doi: 1038/s41586-024-07680-x

Leave a Reply